1) The Rhesus Medicine YouTube channel, in their July 2022 video titled, Depression Explained (Major Depressive Disorder) notes how depression is expected to be the number one cause of disease worldwide by 2030.
2) Roman Gelperin, writing in his book “And it Was All Your Fault: Unraveling the Inner Psychology of Depression” describes how: “Depressed people will often speak of a state of blankness, loneliness, becoming invisible, fading into nothingness, being reduced to zero. They also invariably report feelings of pain and anguish and misery. The emotion of sadness, of course, is nearly always also reported” (Gelperin 12). The state of blankness, loneliness (combined with an intense anxiety and fear of letting others be close), and being reduced to nothing all resonate deeply for me.
3) Vancouver Psychologist Dr Randy Paterson, in his UDEMY course What Is Depression? describes how depression, as an albeit confusing clinical disorder, impacts one’s behaviour, emotions, thoughts, and physiology at different levels during a depressive episode (Paterson - Floating Diamond Model).
4) Paterson also describes how he views depression not as a disease but as more of a syndrome. For Paterson, a disease has generally accepted symptoms whose causes are usually standardized and known, but with a syndrome one has a set of symptoms tend to occur together based on causes that tend to be unique from person to person (Paterson - Major Depressive Episode Criteria).
5) For as long as I can remember, I have always felt this weight of sadness that is the depressive experience bearing over me, even when I was growing up. Having said that, it is important to note that this record is not an attempt to diagnose myself. It is a record of what I have experienced and where appropriate I will reference professional assistance, diagnosis, and support where I have received them.
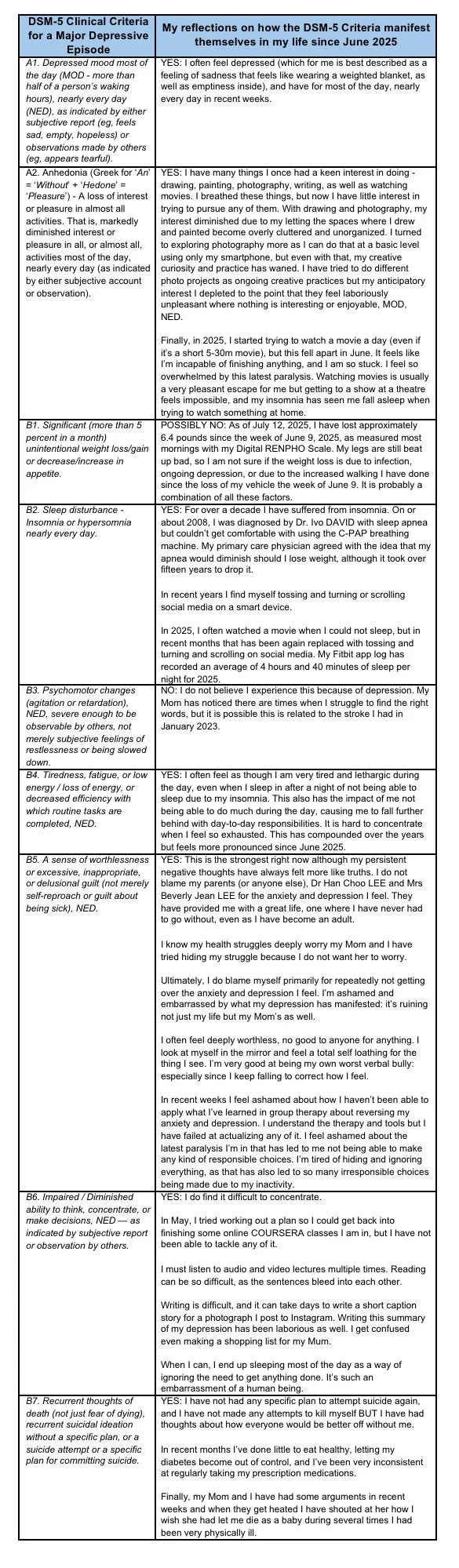
6) The American Psychiatric Association’s Diagnostic and Statistical Manual of Mental Disorders, 5th Edition (DSM-5) outlines the following symptom list for diagnosing a Major Depressive Episode. To be diagnosed, one must meet the cutoff for 5 of the 9 symptoms, where at least one of which must be one of the first 2:
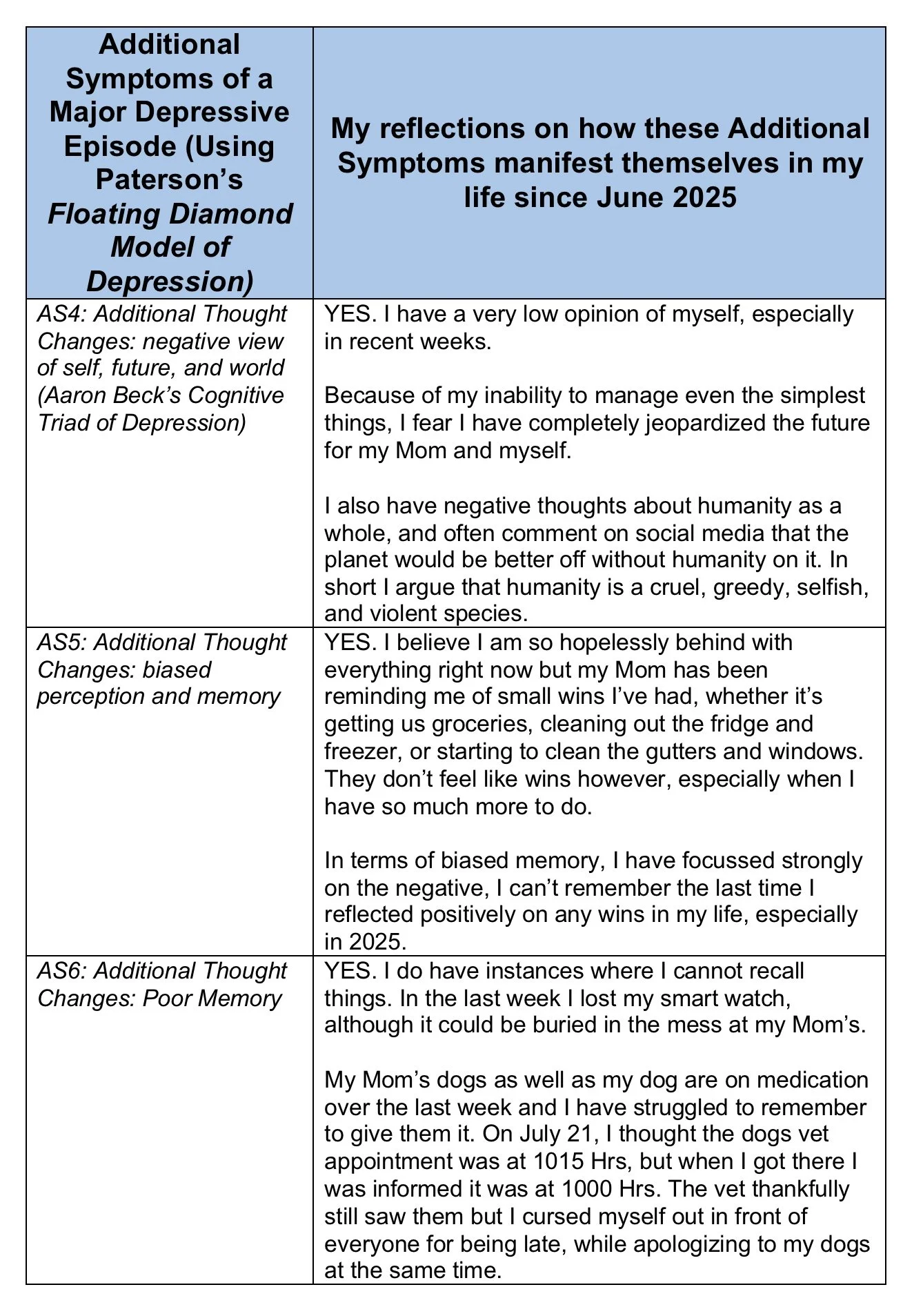
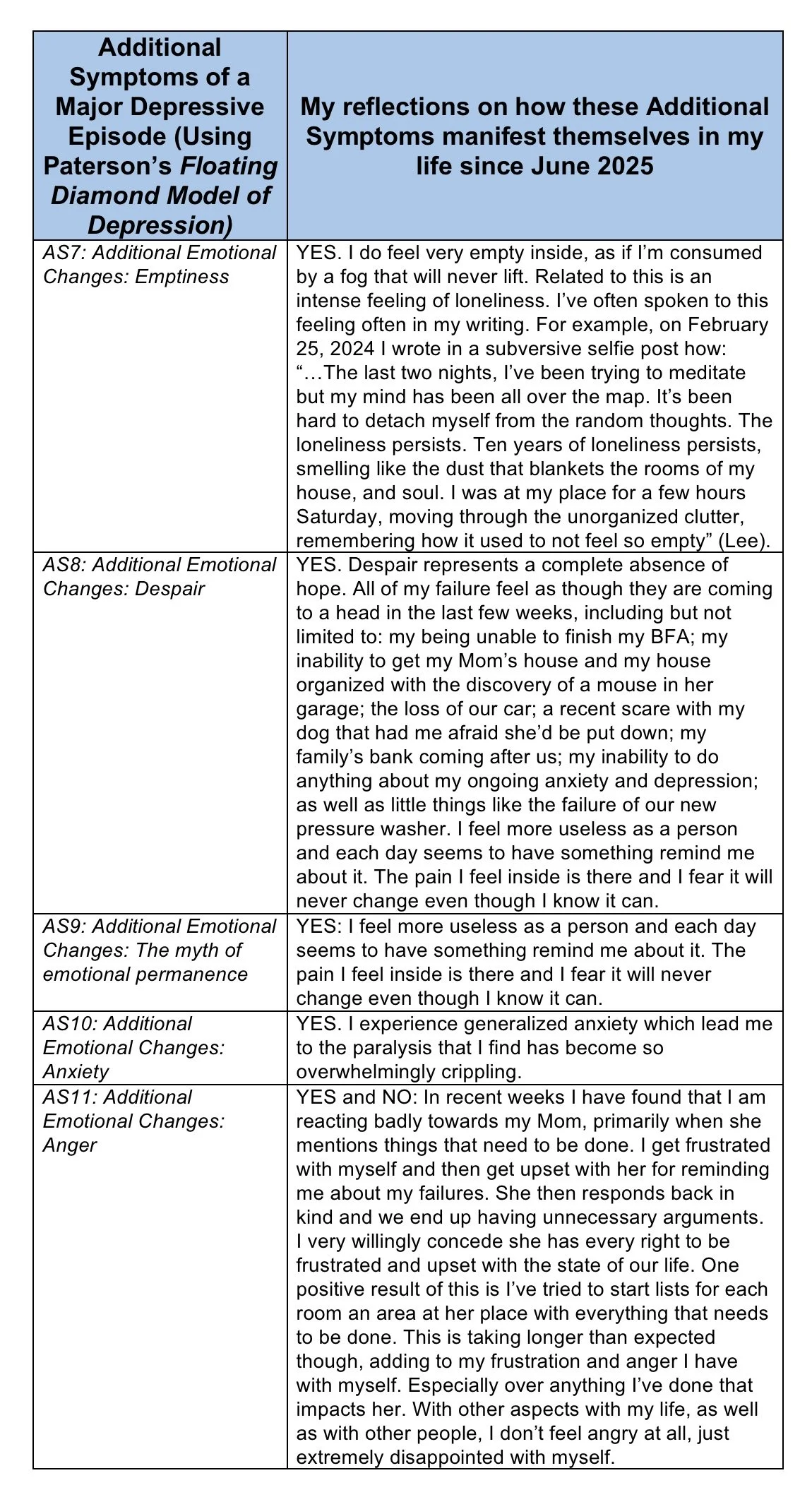
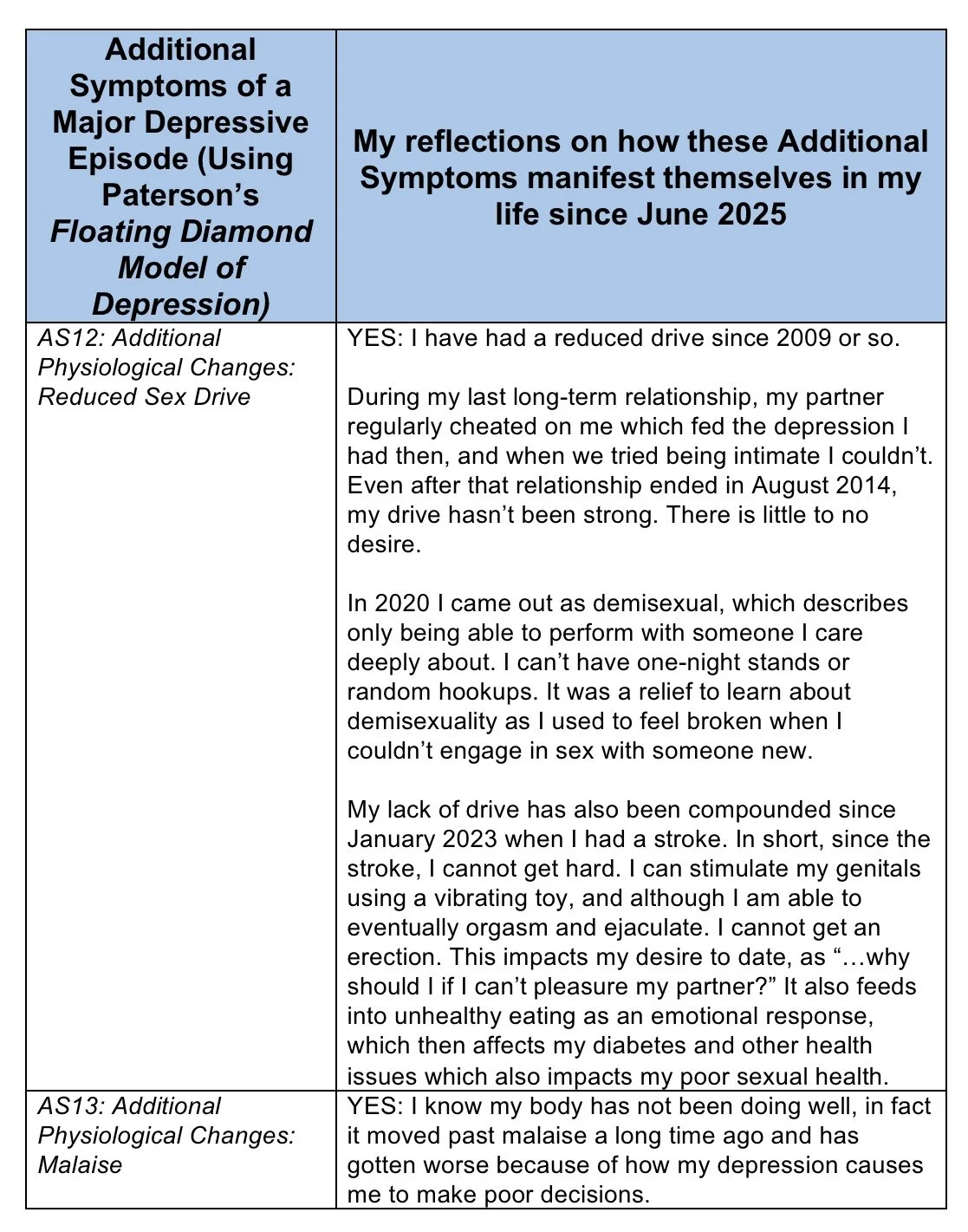
7) Dr Randy Patterson, in his UDEMY course, describes several additional symptoms of depression related to additional behavioural, thought, emotional, and physiological changes that are not necessarily directly addressed by the DSM-5, using his Floating Diamond Model of Depression, as follows:
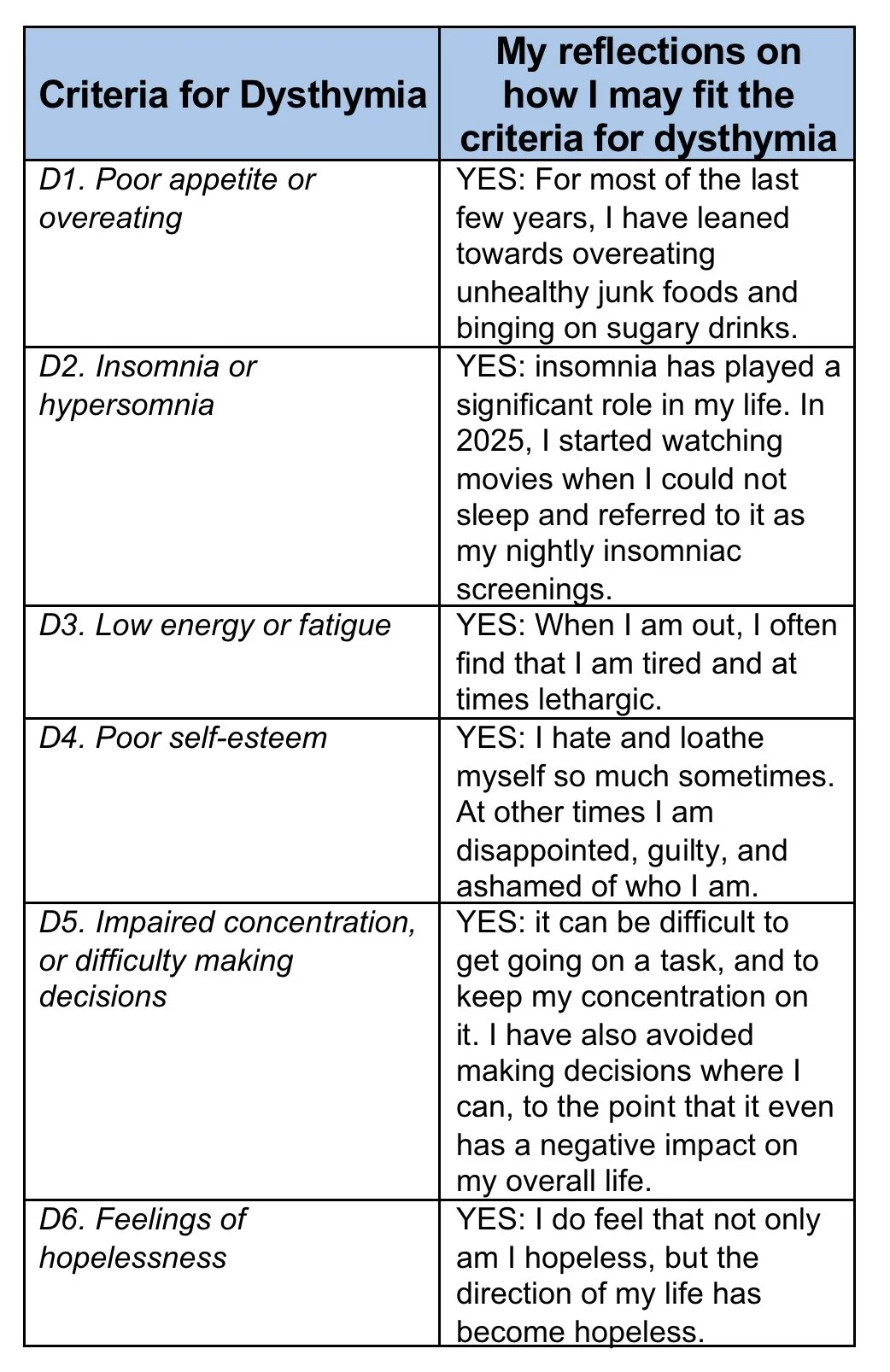
Dysthymia (Persistent Depressive Disorder)
8) Dr Patterson, in his UDEMY course What is Depression? describes dysthymia (persistent depressive disorder) as an ongoing depressed mood that lasts most of the day, more days than not, for at least two (2) years. He describes how a person cannot go for more than two months without symptoms. Furthermore, the problem must cause considerable distress or impairment in a person’s life. Dysthymia also cannot be attributable to a psychotic disorder; underlying medical condition; or the effects of a medication. To qualify as dysthymia, a person also cannot have had manic or hypomanic episodes. Finally, Dr Patterson also notes how individuals require two (2) of the following:
9) In short, I have a low mood, I stay home, avoid seeing others, I have an erratic sleep schedule, I can’t finish many of the things I start, and I don’t eat well or exercise much. My negative self talk and depressive way of thinking has become fairly engrained and even rigid. I have lost the energy I had when I was younger to maintain an interest in and have a positive impact on the world around me.
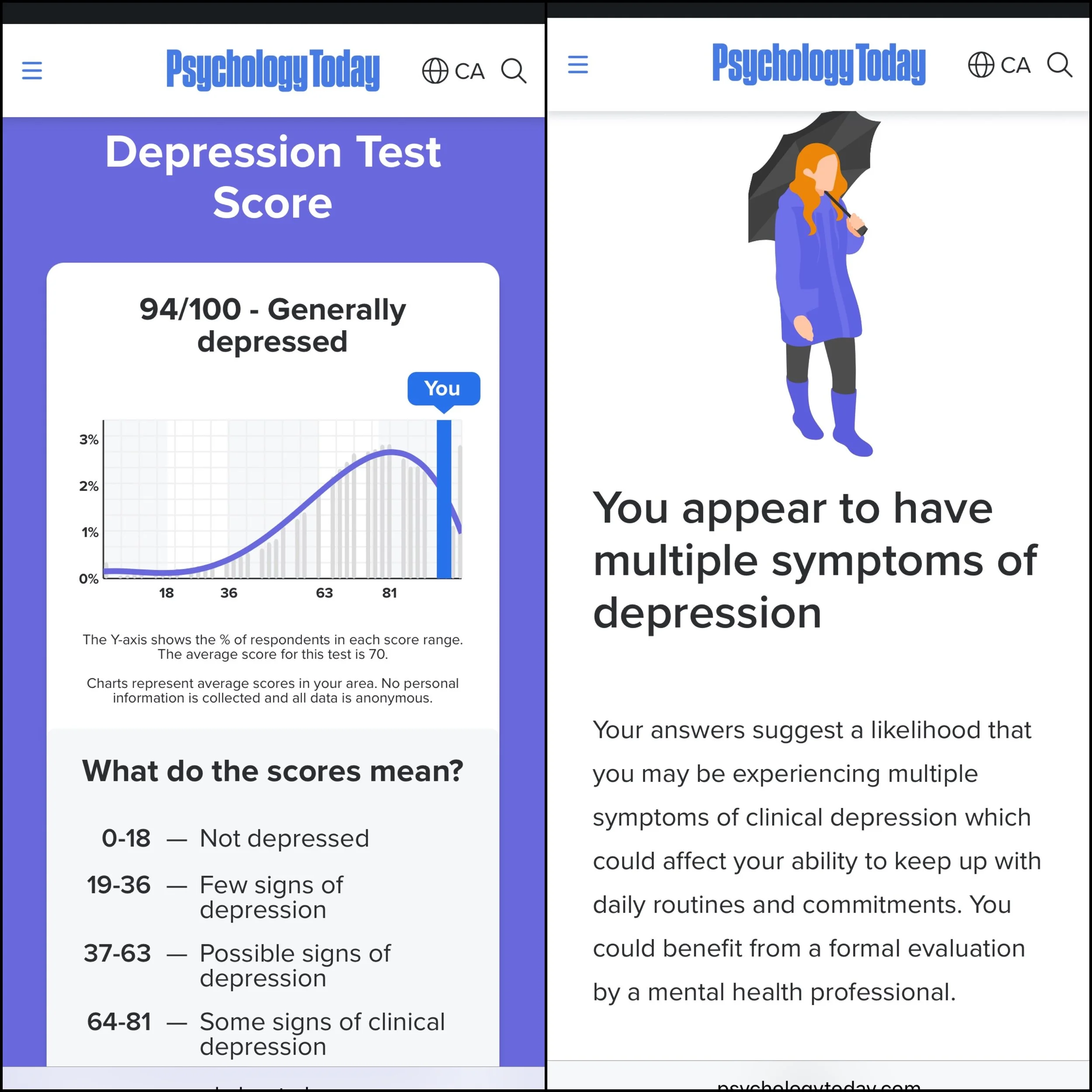
10) On July 15, 2025 I scored 94/100 on Psychology Today’s online Depression Test. It is a twenty (20) question test where one answers the questions based on how strongly they agree or disagree with a statement. Specifically, a score that falls in the range of “82-100” represents one as being generally depressed:
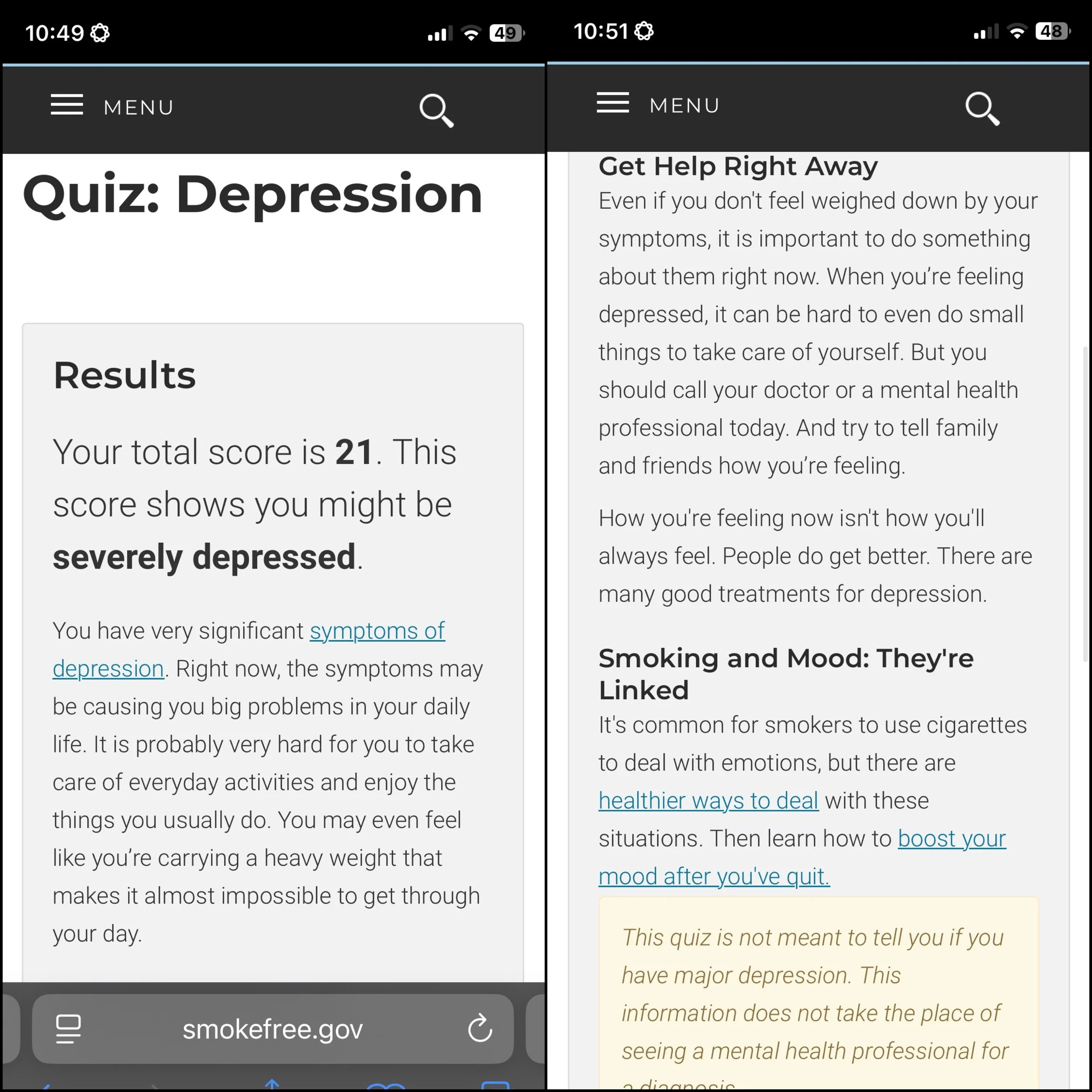
11) On July 25, 2025, I took the US Smoke Free Depression Quiz, adapted from the Quick Inventory of Depressive Symptomatology 16-Item Self-Report (QIDS–SR16) as developed by the University of Pittsburg, on which I scored 21 which highlights that I am likely severely depressed:
12) On July 25, 2025, I took the Yourself 1st website’s mental health assessment and scored 132/180 which the site lists as being of “High Concern,” broken down as follows:
Generalized Anxiety Leading to a Paralysis in Handling Life
13) I also recognize that I have, starting around 2020, likely developed Generalized Anxiety Disorder, which the Safecheck short course, Mental Health in the Workplace defines as being “…an anxiety disorder characterized by excessive and persistent worry about everyday situations and events.” I ultimately deal with my anxiety by ignoring situations that may trigger it.
14) On July 15, 2025, I took the Yourself 1st Anxiety Quiz, and was rated as having moderate anxiety:
15) Specifically, I have found that when I am confronted by a stressful situation that impacts me directly, my mind has a predisposition to go into a frozen state, or paralysis, that makes me to avoid and completely ignore stressful situations, regardless of whatever consequences may arise from me doing that. In other words, I enter the flight mode of the fight-or-flight response (which is also known as the acute stress response) simply because I am paralyzed by fear. My retreat during the day has manifested itself in a kind of bed rotting, one that feeds my anxiety, my insecurities, and the mental decay which leads to rumination the longer I avoid everything. Combined with my sleepless insomniac nights, the bed rotting during the day forms the little sleep I get.
16) The Online Therapy website, in their article Depression and Avoidance Behaviour describes how: “Avoidance plays a major part in dealing with depression and those who sink into major depression are in the grasps of serious avoidance. For many, it can be tempting to effectively give up, and hide away from the world, but the truth is avoidance does nothing but fuel a life that is less enjoyable, less rewarding and more problematic” (Online Therapy). Avoidance has become a dangerously unhealthy part in my everyday life.
17) Sascha Y Struijs et al., in their article, “Approach and avoidance tendencies in depression and anxiety disorders” note how, “Anxiety is linked to increased avoidance and inhibition, whereas depression is linked to decreased approach and diminished behavioral activation” (Sascha Y Struijs et al.). In my experience I have found that I have experienced elements of both.
18) I remember my earlier instances of my choosing to flee stressful situations arose when I was bullied from grades 7-10 in elementary and high school. One aspect of my being bullied involved bullies challenging me to physically fight them “…at the ponds” of a nearby park after school (the bullying ultimately ended when my parents threatened to take my school, its district, as well as the BC Ministry of Education to court. The school issued an edict that anyone who found to be bullying me would be expelled from the school and the school district. So I went from receiving negative attention to none).
19) I remember being put on antidepressants in 2007 by Dr Ivo DAVID after two separate suicide attempts wherein I tried taking my life by overdosing on Tylenol / Tylenol 3. The first instance resulted in nothing happening, and the second instance made me violently ill as my body tried to expel the pills like I had a case of food poisoning. Each time I had taken the pills I had hoped I would simply never wake up again.
20) Since 2020, more recent examples of how this practice of ignoring and fleeing from stressful situations include my inability to:
apply myself consistently to other post secondary courses I have attempted;
communicate effectively with one University professor, Dr Dorothy Barenscott when I fell behind with my work in her courses I attempted to take to complete my Bachelor of Fine Arts, due to my ongoing health issues;
deal with banking and financial matters by keeping in communication with our family’s accountant;
effectively deal with my high blood pressure, insomnia, need to lose weight, type 2 diabetes, and other physical healthcare issues;
effectively actualize coping skills such as CBT and MBSR to improving my life by reducing the instances where I suffer from mental health issues such as anxiety and depression; and
make significant progress on cleaning up and organizing my house as well as my Mom’s.
21) Andrea Darcy, in her March 2023 article for the Harley Therapy Mental Health Blog titled “Avoidance Coping: Is It Adding to Your Anxiety or Depression?” describes how “One way to see coping avoidance is like a fan applied to the flames of your depression or anxiety, sending you in an endless loop. Your very attempt to avoid stress tends to backfire and create more stress. You end up more anxious or depressed then you originally were” (Darcy). As briefly summarized in paragraph 20 above, I have found I’m caught in a snowball effect of a wide assortment of stressors rooted in how I deal with my anxiety and depression.
22) Finally, Dr Theo Tsaousides, writing in his March 2021 article for Psychology Today titled “Fight or Flight: Which is a Better Choice” describes how: “Sometimes, the freeze moment may last seconds, and other times it may last hours, months, even years. When you freeze for too little, you may make impulsive decisions and take careless actions. When you freeze for too long, you may put yourself in a state of endless anxiety, worry, uncertainty, indecisiveness, and procrastination.” My freeze moments definitely last for weeks, months, and even years, thereby contributing to the prolonged periods of depression I experience.
Treatment Overview for Anxiety and Depression
23) Following my 2007 suicide attempts, my primary care physician Dr Ivo DAVID placed me on the antidepressant Citalopram, which I was on intermittently until approximately December 2021 (there were several periods between 2011 and 2017 where I was not on anything, in consultation with Dr DAVID. Although in hindsight, there were times when my depression had not improved but I was too ashamed to admit to it).
24) In 2023 and 2024, I attended several Cognitive Behavioural Therapy groups designed to “…support clients in recognizing triggers, challenging negative thought patterns, and adopting healthy coping methods to manage symptoms.” The specific in-person groups I attended were as follows:
May 1 - July 10, 2023: Anxiety Management Group;
January 25 - April 4, 2024: Depression Management Group; and
August 1 - October 10, 2024: Transdiagnostic Anxiety Management Group.
25) There have been times when I have wondered if I might also be affected by borderline personality disorder. Dr Jordan Peterson has posited that the borderline personality knows exactly what’s wrong but feels incapable or struggles with implementing the solutions that can help mend the borderline personality. As one can see from this letter, I’m aware of what has been ailing me but feel utterly helpless when it comes to resolving any of it. And with this helplessness I’ve been tied to a situation where I fall farther behind with life.
Works Cited
Darcy, Andrea M. “Avoidance Coping – Is It Adding to Your Anxiety or Depression?” Harley Therapy Mental Health Blog, 9 Mar 2023. https://www.harleytherapy.co.uk/counselling/avoidance-coping-depression.htm.
Gelperin, Roman. “And it Was All Your Fault: Unraveling the Inner Psychology of Depression.” The Modern Self Actualization Press, 25 May 2019.
Lee, Steven (@steveleeart). “February 25, 2024 Subversive Selfie Project Post.” Instagram, 25 Feb 2924. https://www.instagram.com/p/C3xH2Y6LxmY/?igsh=NnZlNDV3end0ZXI3.
Paterson, Randy. “Dysthymia (Persistent Depressive Disorder) (Lecture 9)”. What is Clinical Depression?. Udemy, 2014. https://www.udemy.com/share/10dGSl3@eJIuv9kzO3T_6Z2vh7-PczsDeJhEpG4uoAIvnqWkedDWckyyFpMFRGfeCHT028Um/.
Online-Therapy. “Depression and Avoidance Behaviour.” https://www.online-therapy.com/depression/depression-and-avoidance-behavior.
Paterson, Randy. “The Floating Diamond Model - Depression is More Than a Mood Disorder (Lecture 2)”. What is Clinical Depression?. Udemy, 2014. https://www.udemy.com/share/10dGSl3@eJIuv9kzO3T_6Z2vh7-PczsDeJhEpG4uoAIvnqWkedDWckyyFpMFRGfeCHT028Um/.
Patterson, Randy. “Major Depressive Episode - Mood-Related Criteria (Lecture 3)”. What is Clinical Depression?. Udemy, 2014. https://www.udemy.com/share/10dGSl3@eJIuv9kzO3T_6Z2vh7-PczsDeJhEpG4uoAIvnqWkedDWckyyFpMFRGfeCHT028Um/.
Rhesus Medicine. Depression Explained (Major Depressive Disorder). YouTube, 19 Jul 2022. https://youtu.be/tJQRsIbD110?si=7FFYruYm_S1RtBzY&utm_source=ZTQxO.
Struijs, Sascha Y et al. “Approach and avoidance tendencies in depression and anxiety disorders.” Psychiatry research vol. 256 (2017): 475-481. doi:10.1016/j.psychres.2017.07.01
Tsaousides, Theo. “Fight or Flight: Which Is a Better Choice? Understanding the fight-or-flight response and how to deal with it.” Psychology Today, 28 Mar 2021. https://www.psychologytoday.com/us/blog/smashing-the-brainblocks/202103/fight-or-flight-which-is-a-better-choice.